Abdominal wall blocks
Originally from Update in Anaesthesia | www.wfsahq.org/resources/update-in-anaesthesia
Nuria Masip and Steve Roberts* *Correspondence Email: Steve.Roberts@alderhey.nhs.uk
| Summary |
|---|
| Regional anaesthesia is an essential component of paediatric anaesthetic practice. This review describes how to perform the three most common abdominal wall blocks in children: ilioinguinal/ iliohypogastric, rectus sheath and transversus abdominis plane, using either landmark or [if available] ultrasoundguided techniques. |
INTRODUCTION
Regional anaesthesia is an essential component of paediatric anaesthetic practice. Regional blocks allow for a lighter plane of anaesthesia during surgery, and provide excellent pain control after surgery.[1] The aim of this review is to describe how to perform the three most common abdominal wall blocks in children: ilioinguinal/ iliohypogastric, rectus sheath and transversus abdominis plane. We will describe landmark techniques as well as ultrasound-guided techniques. Ultrasound guided blocks are increasingly considered the gold standard as it is possible to identify the anatomy more accurately, which increases the reliability of the block and allows a smaller dose of local anaesthetic to be used. Regional anaesthetic blocks are simple to do, but should be taught by an appropriately skilled mentor. All local anaesthetic blocks should be performed using an aseptic technique; clean the skin with an alcohol-based cleaning solution and wear gloves. Ideally use a short-bevelled block needle for abdominal wall blocks, but a 23G or 21G hypodermic needle may also be used; many advocate ‘blunting’ the tip of the needle on the inside of the cap of the needle to better appreciate the facial planes. All the blocks described should be performed after induction of general anaesthesia.
ILIOINGUINAL/ILIOHYPOGASTRIC NERVE BLOCK (ILNB)
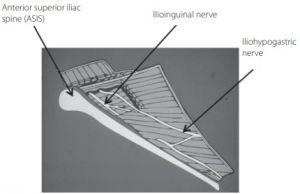
The ilioinguinal/iliohypogastric nerve block (ILNB) provides excellent analgesia after inguinal hernia repair, hydrocele repair and orchidopexy. It does not abolish visceral pain due to peritoneal traction or manipulation of the spermatic cord during inguinal hernia repair or orchidopexy. Bilateral blocks can be used, but it is important to keep the dose of local anaesthetic within safe limits. Perform ILNBs after induction of anaesthesia, before the start of surgery; it is important to make sure that the child is adequately anaesthetised when the cord structures are mobilised, and that additional local infiltration/analgesia is used if a scrotal incision is made. There is much anatomical variation of nerve position between the abdominal wall muscles. The effectiveness of this block can be improved greatly when performed with ultrasound, and lower amounts of local anaesthetic can be used.[2] Anatomy (see Figure 1):
- The iliohypogastric (T12, L1) and ilioinguinal (L1) nerves are terminal branches of the lumbar plexus. They lie deep to the internal oblique.
- The iliohypogastric nerve supplies the gluteal region and the skin over the pubic symphysis.
- The ilioinguinal nerve supplies the area of the skin beneath that supplied by the iliohypogastric nerve and the anterior scrotum.
- The nerves emerge at the lateral border of psoas major and pass anterior to quadratus lumborum. They pierce the lumbar fascia at the lateral border of quadratus lumborum and run in the plane between the internal oblique muscle and transversus abdominis muscles.
- The iliohypogastric nerve pierces (again) the internal oblique and runs under the external oblique superior to the inguinal canal
- The ilioinguinal nerve continues in the inguinal canal.
- In infants the average nerve-peritoneum distance is only 3.3mm[3] .
- The fascial plane between the transversus abdominis muscle and the transversalis fascia is in continuity with the space around the femoral nerve.
Dose
Use a volume of up to 0.5ml.kg-1 0.25% bupivacaine for the landmark technique. In expert hands as little as 0.075 ml.kg-1 0.25% bupivacaine can be effective using ultrasoundguidance; [4] we recommend 0.1-0.2ml.kg-1.
Complications
The most common complication is block failure (more common using the landmark technique). Transient femoral nerve palsy with transient quadriceps paresis may be seen if the injection is too deep. Visceral perforation (colon puncture, small bowel puncture, pelvic retroperitoneal haematoma, bowel haematoma) is associated with poor technique, particularly an injection that is too medial.
Techniques
Landmark technique
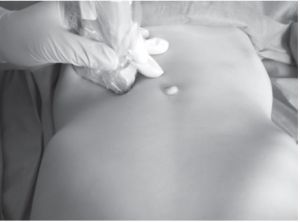
Place the patient supine. Clean the skin over the lower quadrant of the abdominal wall, including the skin over the anterior superior iliac spine (ASIS). Draw up the appropriate dose of local anaesthetic. The needle insertion point is close to the ASIS, approximately 2 - 5mm medial to the ASIS on a line drawn between the ASIS and the umbilicus.[5] Some suggest using the child’s finger as an appropriate guide for the distance from the ASIS to the injection point (NOT the operator’s finger! - see Figure 2). It is important to keep the injection point high, away from the skin crease in the groin where the surgeon will make the incision; otherwise the operating field will be obscured.
Insert the needle just through the skin into the subcutaneous tissues; advance the needle slowly until a fascial ‘click’ or loss of resistance is felt. The click is felt as the aponeurosis of the external oblique is pierced. Aspirate and then inject the local anaesthetic in this position; there is no need to ‘fan’ the injection, and this may increase the incidence of complications.
Ultrasound guided technique
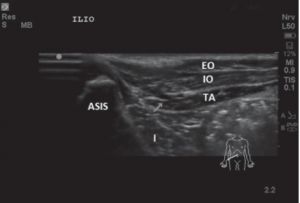
Position the patient supine and clean the skin. Place a high frequency linear probe on the anterior abdominal wall along the line joining the anterior superior iliac spine (ASIS) and the umbilicus (a small footprint probe is useful for infants). (See Figure 3).
The ASIS is the most easily recognizable landmark for this block, it appears as a dark echo-lucent shadow beneath a hyperechoic peak and should be kept at the lateral part of the screen for orientation. Identify (always from the inside out) the peritoneum (hyperechoic line, underneath it you may see peristalsis), transversus abdominis muscle, and internal oblique muscle. The external oblique muscle may not be visible as a distinct muscle layer at this level as it may have become an aponeurosis.
Slide the probe up over the iliac crest, whilst maintaining the same orientation of the probe, to bring all three muscles into view as three distinct layers. This may be useful if there is any doubt about the anatomy and the relevant planes.
The ilioinguinal and iliohypogastric nerves are seen in close proximity to each another as two small round hypoechoic structures with a hyperechoic border. They lie in the plane between the internal oblique muscle and the transversus abdominis muscle close to the ASIS. In children the average distance from the ilioinguinal nerve to the ASIS is 7mm.[4]
Insert the block needle in plane from medial to lateral and ensure that the needle tip is visible at all times as it is advanced. Deposit local anaesthetic around the nerves in the transversus abdominis plane. Note that it may not always be easy to visualise the nerves, in this cause you could place the local anaesthetic in the transversus abdominis plane. If you have any concerns regarding the proximity of your injection to the nerve use a higher volume of local anaesthetic (e.g. 0.2ml.kg-1 0.25% bupivacaine).
RECTUS SHEATH NERVE BLOCK
A rectus sheath block provides intraoperative and postoperative analgesia for mid-line abdominal incisions, for instance, periumbilical surgery (e.g. umbilical hernia repair,[6] paraumbilical hernia repair, epigastric hernia repair), pyloromyotomy, laparoscopic surgery and excision of urachal remnants.
Anatomy
- The rectus sheath encloses the rectus abdominis muscle and is formed by the aponeuroses of the three flat abdominal muscles. These aponeuroses join in the lateral border of the rectus muscle in the point called linea semilunaris.
- Medial to the semilunaris, the aponeuroses split with some fibres passing anterior to the rectus muscle and some posterior:
- The external oblique aponeurosis and the anterior layer of the internal oblique aponeurosis form the anterior wall of the rectus sheath.
- The transversus abdominis aponeurosis and the posterior layer of the internal oblique aponeurosis form the posterior wall of the sheath.
- In the midline the aponeuroses from both sides join to form the linea alba.
- The anterior cutaneous branch of the ventral rami of the inferior six thoracic nerves (T7-T12) run anteriorly through the posterior of the rectus muscle to give off sensory branches to the paraumbilical skin.
- The anterior layer of the rectus sheath is firmly attached to the rectus abdominis muscle at three tendinous intersections (at the level of the xiphoid process, the umbilicus and half-way in between). These tendinous intersections are what separate the muscle into the well-known ‘6-pack’, but it is actually an 8-pack.
- The rectus sheath is loosely attached posteriorly, forming a potential space. Local anaesthetic can spread caudad and cephalad in the plane between the rectus muscle and the posterior rectus sheath.
- Thereis little correlation between the depth of the posterior rectus sheath with age, weight, height or surface area.
- This block is not advisable in neonates without ultrasound guidance as the muscle is so thin and the viscera (especially liver and spleen) are in close proximity.
Dose
Using a landmark technique, use a volume of 0.4ml.kg-1 of 0.25% bupivacaine per side. Using an ultrasound-guided technique a dose of 0.1-0.2ml.kg-1 of 0.25% bupivacaine per side is sufficient.
Complications
Intraperitoneal injection, visceral damage, vascular puncture (it is possible to identify the inferior epigastric vessel in larger children with Doppler).
Techniques
Landmark technique
Use an aseptic technique and draw up the appropriate doses of local anaesthetic. The injection point is just above the umbilicus at the apex of the bulge of the rectus muscle, at 11 o’clock and 1 o’clock to the umbilicus (thinking of the umbilicus as the centre of a clock) (See Figure 5).
Introduce a short-bevelled needle perpendicularly through the skin Advance the needle medially at an angle of 60° towards the umbilicus. Identify the anterior sheath by moving the needle back and forth until a scratching sensation is felt; a pop is felt as the needle passes through the anterior sheath. Advance the needle through the muscle with continued movement of the needle until a scratching is again felt (this indicates the posterior sheath). If there is resistance to injection, it is not sited correctly. Repeat the technique for the opposite side. In children under 10 years of age the rectus muscle is rarely greater than 1cm in thick, therefore when performing this technique the needle should not be inserted any further than this. The depth of the posterior rectus sheath in children is unpredictable, and many advocate using ultrasound for this reason.[7]
Ultrasound technique
Position the patient supine. Select the screen depth (in neonates this will usually be 2cm, infants 3cm, thereafter 4cm). A high frequency linear probe is placed transverse on the abdomen, midline above the umbilicus (see Figure 6). The initial image will have the linea alba in the midline, with a rectus abdominis muscle either side. Posterior to the rectus muscle there are two hyperechoic lines (“train track”): the more superficial one is the posterior part of the rectus sheath and the deeper one is the peritoneum. Use the Doppler to identify the epigastric vessels, although this is not easy in small children (See Figure 7).
Insert the block needle in-plane from lateral to medial. Note it can be difficult to puncture the skin with a block needle (either lift the skin and push the needle through or make a knick in the skin using a sharp bevelled needle). The needle is advanced from lateral to medial, in a shallow trajectory; aim to position the tip of the needle between the rectus muscle and the posterior rectus sheath. Stop the needle tip just superficial to the first white line (the posterior sheath); often a small ‘give’ is felt as you come out of the muscle into the potential posterior space. The needle is positioned correctly if the rectus sheath peels away from the muscle during injection of the local anaesthetic. Deposit local anaesthetic in this potential space between the rectus abdominis muscle and the posterior rectus sheath. In neonates you could use saline to identify the correct plane, avoiding the waste of the limited local anaesthetic. Note that in small children it is possible to use a large footprint probe in the midline and block both sides without adjusting the probe. Spread of the local anaesthetic after injection can be assessed by turning the probe into a paramedian longitudinal plane.
TRANSVERSUS ABDOMINIS PLANE BLOCK (TAP) BLOCK
The standard transversus abdominis plane (TAP) block provides intraoperative and postoperative analgesia for lower abdominal incisions. A subcostal TAP block can be provide analgesia for abdominal surgery above the umbilicus. TAP block can be performed unilaterally (e.g. inguinal hernia repair), or bilaterally (e.g. for laparoscopic surgery). It may be used as an alternative to an epidural, but it does not provide visceral analgesia; it should be performed after induction of anaesthesia, and adequate anaesthesia should be provided during visceral manipulation. A comprehensive review of the transversus abdominis plane (TAP) block can be found in WFSA ATOTW 239.[8]
A TAP block is ideally used for inguinal hernia repair, colostomy formation, appendectomy (laparoscopic and open techniques), iliac crest bone graft harvesting, laparoscopic cholecystectomy, and laparoscopic nephrectomy or to provide analgesia after renal transplant.
Anatomy
- The skin of the anterior abdominal wall is supplied by the ventral rami of the inferior six thoracic spinal nerves (T7 to T12).
- In the lateral part of the anterior abdominal wall there are 3 muscle layers, from deep to superficial they are: the transversus abdominis muscle (TA, it is the most internal of the 3 muscle layers), the internal oblique muscle (IO, it is positioned in-between TA and EO) and the external oblique muscle (EO, it is the largest and most superficial of the 3 muscles).
- The ventral rami of T 7 to T12 run in the plane between the transversus abdominis muscle and the internal oblique muscle: the transversus abdominis plane (TAP).
Dose
Use a volume of 0.3 – 0.5ml.kg-1 of 0.25% bupivacaine per side.
Techniques
The landmark technique is not recommended in children due to the danger of visceral damage and is therefore not described here. If ultrasound is not available, in terms of risk/benefit, other techniques such as simple infiltration with local anaesthetic are preferable.
Ultrasound-guided mid-axillary TAP block
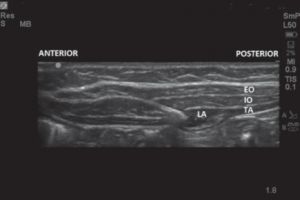
Position the patient supine. Place a high frequency linear ultrasound probe in a transverse plane between the iliac crest and the costal margin. Start scanning from the linea alba in the midline, then move laterally until the probe is between the iliac crest and the costal margin (See Figure 8).
Identify the peritoneum and then the abdominal muscles: transversus abdominis, internal oblique, and external oblique. In obese children fascial planes may be present within the adipose tissue, this can lead to misidentification of the muscle layers; therefore always identify the muscle layers from deep to superficial.
The target is the fascial plane between the transversus abdominis and the internal oblique muscles. Advance the needle in an antero-posterior direction (See Figure 8). Aim to puncture the fascia on the deep aspect of the internal oblique muscle layer (a slight give or pop is often felt) (See Figure 9).
In neonates the muscles are less developed and therefore differentiation between the layers can be difficult to the inexperienced practitioner. The injection is seen as a neat lens-shaped deposit of local anaesthetic forming between the transversus abdominis muscle and the fascia separating the internal oblique muscle and transversus abdominis. If you are concerned that the local anaesthetic dose may be wasted whilst identifying the correct plane, use saline to identify the correct plane before injecting the local anaesthetic dose.
In older children it may prove difficult to enter the TAP. Guide the needle very carefully into the transversus abdominis muscle, then slowly withdraw the needle as an assistant injects; as the needle enters the correct position, local can be seen spreading through the plane.
Ultrasound guided subcostal approach
Position the patient supine. Place high frequency linear ultrasound probe in an oblique transverse plane, parallel to the subcostal margin (lateral to the rectus sheath). Identify the medial border of the external oblique, internal oblique and transversus abdominis muscles. Subsequently identify the TAP in between these inner two muscles. Insert the needle at the lateral edge of rectus abdominis muscle. Advance the needle in-plane away from the midline and parallel to the costal margin; use the local anaesthetic to hydrodissect the plane, carefully advancing the needle into the space created. Repeat this process until the anterior 2/3 of the subcostal margin has been covered.
Complications
Peritoneal perforation, organ perforation (in neonates the liver and spleen are particularly prominent). The TAP block has a higher rate of complications than other blocks in children.[9]
FURTHER READING
http://www.euroespa.com/science-education/specializedsections/us-regional-anaesthesia/
REFERENCES
- ↑ Boretsky KR. Regional anesthesia in pediatrics: marching forward. Curr Opin Anaesthesiol. 2014; 27: 556-560.
- ↑ van Schoor AN, Boon JM, Bosenberg AT, Abrahams PH, Meiring JH. Anatomical considerations of the pediatric ilioinguinal/ iliohypogastric nerve block. Paediatr Anaesth. 2005; 15: 371- 377.
- ↑ Willschke H, Marhofer P, Bosenberg A et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005; 95: 226-230.
- ↑ 4.0 4.1 Willschke H, Bosenberg A, Marhofer P et al. Ultrasonographicguided ilioinguinal/iliohypogastric nerve block in pediatric anesthesia: what is the optimal volume? Anesth Analg. 2006; 102: 1680-1684.
- ↑ Weintraud M, Marhofer P, Bosenberg A et al. Ilioinguinal/ iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg. 2008; 106: 89-93.
- ↑ Flack SH, Martin LD, Walker BJ et al. Ultrasound-guided rectus sheath block or wound infiltration in children: a randomized blinded study of analgesia and bupivacaine absorption. Paediatr Anaesth. 2014; 24: 968-973.
- ↑ Willschke H, Bosenberg A, Marhofer P et al. Ultrasonographyguided rectus sheath block in paediatric anaesthesia--a new approach to an old technique. Br J Anaesth. 2006; 97: 244-249.
- ↑ Russon K et al. Transversus abdominus plane block. WFSA Anaesthesia Tutorial of the Week 2011 No. 239. http://www.wfsahq.org/components/com_virtual_ library/media/ea51ff0934644a9e41bcf82f65a96a58- 474f4fcc0e20052dd9ed683ca9995db2-239-TransversusAbdominus-Plane-Block.pdf
- ↑ Long JB, Birmingham PK, De Oliveira GSJ, Schaldenbrand KM, Suresh S. Transversus abdominis plane block in children: a multicenter safety analysis of 1994 cases from the PRAN (Pediatric Regional Anesthesia Network) database. Anesth Analg. 2014; 119: 395-99.