Upper and lower limb blocks in children
Originally from Update in Anaesthesia | www.wfsahq.org/resources/update-in-anaesthesia
Adrian Bosenberg Correspondence Email: adrian.bosenberg@seattlechildrens.org
Adrian Bosenberg Professor, Department Anesthesiology and Pain Management, Faculty Health Sciences, University Washington, Seattle, USA Director Regional Anesthesia Seattle Children’s Hospital 4800 Sandpoint Way NE Seattle, WA 98105 USA
| Summary |
|---|
| This article outlines regional anaesthetic techniques and methods used to identify and block individual nerves to provide analgesia for surgical procedures of the upper and lower limbs. Expertly performed, peripheral nerve blocks can provide long lasting anaesthesia and analgesia for surgery or after injury to the upper or lower limbs in children. Specific knowledge is required for the indication, technique and dose of local anaesthetic for each block. A safe dose of local anaesthetic must be used at all times, and care taken to avoid inadvertent intravascular injection of local anaesthetic. The differences between adults and children are highlighted together with techniques to improve the success of blocks. |
INTRODUCTION
Regional anaesthesia is commonly used as an adjunct to general anaesthesia and plays a key role in the multimodal approach to perioperative pain management in children.[1],[2] Peripheral nerve blockade has increased with the development of age-appropriate equipment, safer, long-acting local anaesthetic agents, increasing experience and low complication rates.
The safety of peripheral nerve blocks in children has been established in large-scale prospective studies, although caudal epidural remains the most popular and frequently used block in infants and small children.[3],[4],[5] The experience of the operator, pathology, the site and extent of surgery, the child’s body habitus and the presence of contractures will dictate the final choice of technique.
This article outlines regional anaesthetic techniques and methods used to identify and block individual nerves to provide analgesia for surgical procedures of the upper and lower limbs. The differences between adults and children are highlighted together with techniques to improve the success of blocks.
METHODS TO IMPROVE ACCURACY OF PERIPHERAL NERVE BLOCKS
Peripheral nerve blocks, particularly in young children, can be challenging because anatomical landmarks are poorly defined and vary with age. Successful peripheral nerve blocks require an awareness of these differences, knowledge of developmental anatomy and an understanding of the equipment used.
Most children are sedated or under general anaesthesia when nerve blocks are performed. Ultrasound guidance is preferable when available. A peripheral nerve stimulator and insulated needles are the next best option although successful blocks can be achieved with non-insulated needles.[6]
Nerve stimulator
Many peripheral nerve stimulators are available. Familiarise yourself with a particular device and stick with it. Read the manufacturer’s instructions and understand how the nerve stimulator works before you use it.
The following basic principles should be followed to locate a peripheral nerve or plexus accurately:
- Muscle relaxants must be withheld until after completion of the block.[7]
- Attach the Negative electrode to the Needle and the Positive electrode to the Patient using a standard ECG electrode.
- Set the initial peripheral nerve stimulator output to 1-1.5 mA at 1-2 Hz for 0.1msec. Advance the needle through the skin and underlying tissue planes until you elicit nerve-specific muscle contractions distally.
- Decrease the current output and adjust the needle location until you see maximum motor response with least current i.e. at approximately 0.3-0.5mA.
- Aspirate and inject local anaesthetic (provided no blood returns when you aspirate as this implies the needle tip is within a blood vessel) - muscle twitches will stop immediately indicating a successful block is likely. If this does not happen you must reposition the needle and repeat the process.
- Do NOT inject local anaesthetic if you find vigorous muscle contraction at <0.2mA or resistance to injection. Both suggest intraneural injection, and nerve damage could result.
Surface nerve mapping
This is a modification of the standard nerve stimulator technique.[8] The path of a superficial motor nerve (or plexus) can be traced by stimulating the motor component of the nerve transcutaneously. The nerve stimulator output is set at 2-5mA at 1-2Hz and the negative electrode used as the “mapping electrode”. The current required varies and is dependent on the depth of the nerve and the skin moistness. Mark the point at which maximal motor response is elicited. This serves as the surface landmark for that block. Excess pressure applied over the nerve may inhibit the response. Direct muscle stimulation is finer and more localized.
The ‘nerve mapping technique’ may be used for:
• The brachial plexus (supraclavicular, axillary)
• Musculocutaneous, ulnar, median and radial nerve blocks of the upper limb
• Femoral, sciatic and popliteal nerve blocks in the lower limb.
Surface nerve mapping is particularly useful where anatomical landmarks are difficult e.g. children with arthrogryposis or congenital limb defects.
Ultrasound guidance
This has become an important adjunct in regional anaesthesia; although anaesthesia departments in low- and middle-income countries (LMIC) may not be able to make this expensive item a priority.[9],[10],[11],[12],[13] Using real time ultrasound imaging, correct needle and local anaesthetic placement around the nerve can be verified and thus the risk of intraneural or intravascular injection reduced. Detailed descriptions of ultrasound-guided blocks can be obtained from recent review articles.[10],[11],[12],[13]
UPPER LIMB BLOCKS
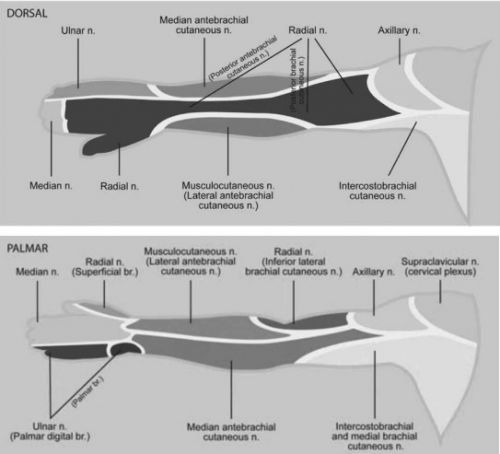
The motor and sensory innervation of the whole upper extremity is supplied by the brachial plexus, with the exception of part of the shoulder (innervated by the cervical plexus), and the sensory innervation to the medial aspect of the upper arm (supplied by intercostobrachial nerve, a branch of the 2nd intercostal nerve).
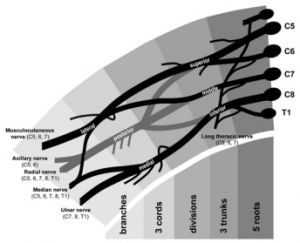
Anatomy of the brachial plexus (see Figure 1)
The anterior primary rami of C5-8 and the bulk of T1 form the brachial plexus. These five roots emerge from the intervertebral foramina to lie between the scalenus anterior and scalenus medius muscles (which attach to the anterior and posterior tubercles of the transverse process of the cervical vertebrae respectively).
The fascia of these muscles encloses the plexus in a sheath that extends laterally into the axilla. A single injection of local anaesthetic within this sheath produces complete plexus blockade by blocking the trunks (supraclavicular approaches) or the cords (infraclavicular approaches). As the spinal roots pass between the scalenus muscles they unite to form three trunks - upper C5-C6; middle C7; lower C8-T1. Emerging from the interscalene groove, the three trunks pass downward and laterally to lie postero-lateral to the subclavian artery as it crosses the upper surface of the first rib. The subclavian artery is not easily palpable above the clavicle in children. At the lateral border of the first rib, each trunk divides into anterior and posterior divisions, which then join to form the lateral, medial and posterior cords, named according to their relationship to the axillary artery. These cords then divide into the nerves of the brachial plexus – musculocutaneous, ulnar, median and radial.
Many anatomical landmarks used in adults maybe difficult to feel in anaesthetised children, particularly infants8 . The scalenus muscles are poorly developed making the interscalene groove difficult to delineate. The subclavian artery is seldom palpable above the clavicle in infants and preadolescent children.
The brachial plexus can be blocked at various levels, the choice depending on the planned surgical procedure, the experience of the provider and anatomical variants (See Table 1).[12],[13]
Interscalene approach Although the interscalene approach has been used for shoulder and elbow surgery in children, this approach must be used with caution.[14] Potential complications include intravascular injection, intrathecal injection, pneumothorax (reported incidence in children is low), Horner’s syndrome and temporary phrenic nerve palsy.
| Neck | Interscalene
Parascalene Supraclavicular |
| Infraclavicular | |
| Axillary | Perivascular approach
Transarterial approach |
Supraclavicular approach
This is indicated for all upper extremity surgery, particularly if the shoulder is involved. Position: Supine, pillow under shoulders, arm extended along side the body, head turned to opposite side.
Landmarks:
Clavicle-mid point, transverse process of C6 (Chassaignac’s tubercle), posterior border sternocleidomastoid, cricoid cartilage, brachial plexus.
Dose:
0.2-0.3ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine. Lower concentrations reduce the degree of motor block.
Technique:
With the patient correctly positioned, the components of the brachial plexus become more superficial and are easily palpable in most children. The site of puncture is at the junction of the middle and lower third of a line joining Chassaignac’s tubercle to the midpoint of the clavicle (if Chassaignac’s tubercle cannot be palpated extending a line from the cricoid cartilage to posterior border of sternocleidomastoid should suffice).
Alternatively, insert an insulated needle perpendicular to the skin at the site where maximal distal muscle twitches (usually flexion or extension at the elbow) is ‘mapped’ or simply over the point where the brachial plexus can be palpated.
Complications:
Success rate is high. Complications caused by faulty technique include pneumothorax, vascular puncture, Horner’s syndrome and phrenic nerve palsy.[14] Nerve damage is possible with injudicious injection against resistance but the possibility of surgical damage should always be excluded.
Axillary approach
The axillary block is the most popular brachial plexus block in children.[14],[15],[16],[17] It is relatively safe and provides good analgesia for surgery of the forearm and hand. The risk of complications is low. The main limitation is incomplete block of the shoulder and lateral aspect of the forearm onto the thenar eminence (musculocutaneous nerve sensory distribution). Axillary block may be used for a variety of procedures on the hand and forearm (particularly on the medial aspect), such as open reduction with internal fixation of a forearm fracture, closed reduction of forearm fractures, congenital hand anomalies (syndactyly repair), treatment of vascular insufficiency or finger re-implantation.[16],[17]
Perivascular approach
Position:
Supine, arm abducted 90º, elbow flexed, hand behind head.
Landmarks:
Pectoralis major, the coracobrachialis muscle, axillary artery.
Dose:
0.2-0.5ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine. Lower concentrations reduce the degree of motor block.
Technique:
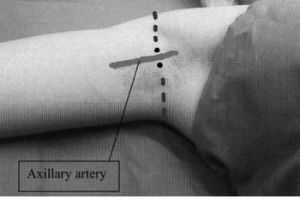
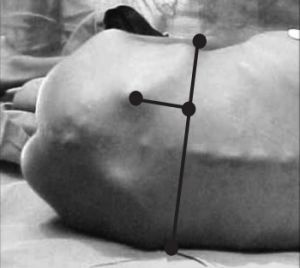
Palpate the axillary artery as high as possible in the axilla in the tissues overlying the humerus at the junction of the lower border of pectoralis major and coracobrachialis muscles (see Figure 2). If using a nerve stimulator technique, introduce an insulated needle immediately superior to the pulsation at a 45-60° angle to the skin and direct parallel to the artery towards the midpoint of the clavicle with the nerve stimulator set at 1mA.[18] Distal muscle twitches are elicited, usually in the median or radial nerve distributions, as the sheath is penetrated. Gradually reduce the output of the nerve stimulator to approximately 0.3-0.4mA while the muscle twitch is maintained, adjust the position of the needle as needed. Local anaesthetic solution can then be injected.
Alternatively, use a nerve stimulator set at 3-5mA to map the median nerve, radial and ulnar or musculocutaneous nerves transcutaneously in the axilla on either side of the arterial pulsation. Insert an insulated needle at the point of maximum muscle twitch.
A cannula-over-needle technique can be used to cannulate the brachial plexus sheath in the axilla using a landmark technique. The axillary artery is located as described above, and a 22G cannula is inserted at 30º to the skin, anterior to the artery and in a line parallel to the pulsation of the axillary artery.17 The cannula is passed over the needle after feeling a ‘click’ when the cannula pierces the axillary sheath. Check for negative aspiration of blood and inject 0.5ml.kg-1 0.25% plain bupicavaine.
Whichever technique is used, distal pressure applied during and immediately following injection will facilitate proximal spread and blockade of the musculocutaneous nerve.
The musculocutaneous nerve may be blocked separately to provide analgesia for procedures involving the lateral forearm. Advance a needle, introduced perpendicularly to the skin just above the axillary pulsation, into the coracobrachialis muscle until forearm flexion is elicited using a nerve stimulator. Inject 0.5-1ml local anaesthetic just deep to the fascia.
Complications are rare but include hematoma from accidental vascular puncture; in this event apply pressure for at least 5 minutes.
Infraclavicular approach
Position:
Supine, pillow under shoulders, head turned to opposite side, upper arm adducted alongside body, elbow flexed to 90° with forearm placed on abdomen.
Landmarks:
Clavicle-lower border, coracoid process of scapula, axillary artery as it emerges beneath clavicle.
Dose:
0.2-0.3ml.kg-1 0.25-0.5% bupivacaine, 1-2% lignocaine. Lower concentrations reduce the degree of motor block.
Technique:
A number of approaches have been described.[18],[19],[20]With the child positioned correctly, divide the clavicle into three parts. Make a mark at the point where the pulse is felt as it emerges below the clavicle, or where any distal flexion or pronation is “mapped”. Insert a needle infra-clavicularly at the junction of the middle and lateral third of the clavicle and directed towards this mark. The needle passes lateral to the cupola of the lung and is unlikely to encounter the lung along its course. Seek pronation or flexion at the elbow. Once the nerve is located, reduce the voltage on the nerve stimulator to 0.2 to 0.3mA.
Alternatively, insert the needle at the midpoint of the lower border of the clavicle at 45-60° angle and direct towards the axilla in the same manner until distal muscle twitches are elicited.
A vertical infra-clavicular approach using the coracoid process as a landmark has also been described in children.[18],[19],[20] The site of puncture is 1-2cm caudad and 0.5-1cm lateral to the coracoid process in the lower part of the delto-pectoral groove. Insert the needle perpendicular to the skin until distal muscle twitches are elicited.
Location of the brachial plexus may be difficult in some patients and ultrasound guided approach has been recommended.[12],[21] Proponents of this technique claim more effective sensory and motor block than with the axillary approach.[20],[21][22]
Elbow blocks
Median nerve
Indication:
Surgery on volar aspect of the forearm and the palmar portion of the hand.
Position:
Supine, arm extended, elbow slightly flexed to accentuate the tendons of the biceps and the brachioradialis.
Landmarks:
Cubital fossa, brachial artery, biceps tendon.
Dose:
0.1-0.2ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine.
Anatomy:
The median nerve in the cubital fossa is located medial to the brachial artery and the biceps tendon beneath the deep fascia.
Technique:
After ‘surface mapping’ the median nerve, insert an insulated needle medial to the pulsation of the brachial artery. Pronation of the arm with opposition of the fingers is noted when the median nerve is stimulated.
Ulnar nerve
Indication:
For surgery in the ulnar distribution of the hand including the medial aspect of the hand and fingers
Position:
Supine, elbow flexed 90°, arm on chest with hand on opposite shoulder.
Landmarks:
Olecranon groove.
Dose:
1-2ml 0.25-0.5% bupivacaine, or 1-2% lignocaine.
Anatomy:
The ulnar nerve lies in the groove posterior to the medial condyle of the humerus midway between the olecranon and the medial epicondyle.
Technique:
The ulnar nerve can be blocked at the olecranon groove. A small volume of 0.25% bupivacaine is injected into the area.
Complications:
Nerve injury, compression of the nerve.
Radial nerve
Position:
Supine, elbow slightly flexed.
Landmarks:
Biceps tendon, lateral condyle of humerus.
Dose:
1-2ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
Technique:
Identify lateral condyle of humerus and tendon of the biceps muscle. The radial nerve lies adjacent to the condyle, lateral to the biceps tendon. With the arm slightly flexed at the elbow, the radial nerve can be stimulated with a mapping probe in this position. Movement of the thumb confirms the location and small volume of local anaesthetic can be injected at that point.
Musculocutaneous nerve in the forearm
Position:
Arm extended or arm on abdomen.
Landmarks:
Lateral condyle of humerus.
Dose:
1-2ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
The musculocutaneous nerve courses superficially along the lateral aspect of the forearm where it can be mapped along most of its course. A superficial ring of local anaesthetic solution (0.1ml.kg-1) injected at the distal end of the lateral condyle of the humerus along the pronator teres muscle should block the musculocutaneous nerve.
Wrist blocks
An appropriate nerve block at the wrist may be used to provide analgesia for children undergoing minor surgical procedures on the hand or fingers. The nerves that can be blocked at this level are the median, ulnar and radial nerves. Small volumes of local anaesthetic (1-2ml) can provide good analgesia for a number of hours.
Median nerve
The median nerve is the major nerve supplying the hand and therefore most surgical procedures of the hand will require a median nerve block at least.
Position:
Hand pronated.
Landmarks:
Palmaris longus tendon. Volar aspect wrist
Dose:
0.5-1ml 0.25-0.5% bupivacaine or 1-2%lignocaine.
Anatomy:
The median nerve lies within a fascial sheath between palmaris longus tendon and flexor carpi radialis. Surface nerve mapping at this point will elicit opposition of the thumb. A sheath that communicates with the neurovascular bundle is located at the ulnar aspect of the palmaris longus tendon. Complications: Rare - carpal tunnel syndrome or injury to the median nerve can be avoided by restricting the volume of local anaesthetic used.
Radial nerve
Position:
Hand supinated.
Landmarks:
Anatomical ‘snuff box’, styloid process-radius, radial artery.
Doses:
1-2ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
Anatomy:
The radial nerve at the wrist is purely sensory and thus nerve mapping is not possible. Just above the styloid process, the radial nerve divides into two branches, one supplying dorsum of the hand and another supplying the thenar eminence and 1.5 fingers.
Technique:
The nerve lies superficial proximal to the ‘anatomical snuff box’. Inject a wheal subcutaneously starting lateral to the radial artery on the lateral aspect of the wrist using a fine needle.
Ulnar nerve
Position:
Hand supinated.
Landmarks:
Flexor carpi ulnaris tendon, ulnar artery. Dose: 1-2ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
Anatomy:
The ulnar nerve is located in the palmar sheath immediately lateral to the flexor carpii ulnaris tendon but medial to the ulnar artery. “Mapping” at this point will elicit flexion of the little finger. Inject into this area to provide analgesia for surgery on the ulnar aspect of the hand and the medial 1.5 fingers.
Bier’s block or intravenous regional anaesthesia
Bier’s block or intravenous regional anaesthesia (IVRA) is performed by introducing local anaesthetic into a limb isolated by means of tourniquet. IVRA is suitable for short (<30min) surgical procedures on the distal arm or leg or reduction of fractures in older children. Operating time is limited by tourniquet pain (30-40 min).
Equipment:
Single or double cuff tourniquet cuff, IV cannula, monitors.
Drugs:
10-40ml 0.5% lignocaine or prilocaine depending on limb and size of patient. Maximum safe dose: lignocaine 3mg.kg-1; prilocaine 6mg.kg-1
Technique:
Set up monitors (ECG, BP, SpO2 ) and insert an IV cannula as distal as possible in the limb to be operated upon. Insert a second cannula into the opposite arm for IV access in case of emergency. Elevate the limb for several minutes to exsanguinate. Inflate the tourniquet 50-100mmHg above systolic BP and ensure the cuff does not leak. Inject the local anaesthetic slowly via the IV cannula. Surgery may proceed after about 5 minutes. The tourniquet must remain inflated for a minimum of 20 minutes from the time of local anaesthetic injection. At the end of the procedure the cuff can be deflated - closely observe the patient for at least 10min for signs of toxicity. IVRA is generally safe provided the tourniquet cuff does not leak or accidentally deflate. A purpose made ‘double cuff’ may be used to increase the safety of this technique and to manage pain from the tourniquet (see http://www.nysora.+com/techniques/3071-bier-block.html).
LOWER LIMB BLOCKS
Most lower extremity procedures can be performed under a caudal block (see article p88). Peripheral nerve blocks are more specific and confined to the site of surgery, the duration of analgesia is longer and the potential side effects of neuraxial blockade can be avoided (bilateral motor weakness, urinary retention).[23],[24],[25]
Anatomy of the lumbar and sacral plexus
Motor and sensory innervation of the lower extremity is supplied by the lumbar and sacral plexus. The lumbar plexus is derived from the anterior primary rami of lumbar nerves L1- L4 and a variable contribution from T12 and L5. The lumbar plexus is located anterior to the transverse processes of the lumbar vertebrae within the psoas major muscle. The psoas compartment is bordered posteriorly by quadratus lumborum and anteriorly by psoas major. The femoral nerve, lateral cutaneous nerve of thigh, and obturator nerve are branches of the lumbar plexus and supply the majority of the upper leg including the thigh and its lateral aspect. The saphenous nerve provides sensory innervation below the knee to the medial aspect of the lower leg and foot. (See Table 2 and Figure 4)
The sacral plexus is derived from the anterior primary rami of L5, S1-S3 with contributions from L4 and S4. The plexus lies anterior to the piriformis muscle behind the pelvic fascia on the posterior wall of the pelvic cavity. The sciatic nerve is derived from the sacral plexus to supply the knee, the leg and most of the foot except for the medial aspect supplied by the saphenous nerve. A proximal branch of the sciatic nerve, the posterior cutaneous nerve of the thigh, supplies the posterior aspect of the thigh and the hamstring muscles.
| Lumbar plexus block | |
| Femoral nerve | |
| Lateral cutaneous nerve of thigh | |
| Sciatic nerve | Posterior approach
Infragluteal approach Popliteal fossa approach |
| Ankle block |
Lumbar plexus block
The lumbar plexus can be blocked within the psoas muscle at the level of the transverse process of L4. In children the transverse process is not fully developed and using the transverse process as a guide usually places the needle too medial and increases the risk of complications, i.e. spinal anaesthesia secondary to puncture of the dural cuff on the spinal roots, or retrograde epidural spread to opposite side.
Indications:
Unilateral block of the hip (congenital dislocation of hip), thigh (open reduction and internal fixation of femoral fractures) or knee surgery.
Position:
Lateral position, hips and knees flexed.
Landmarks:
Posterior superior iliac spine, intercristal line, spinous process L4. Dose: 0.5ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine.
Technique:
With the child in position, insert an insulated needle perpendicular to the skin where a line drawn from the posterior superior iliac spine (PSIS) parallel to the spinous processes of the vertebrae intersects the intercristal (Touffier’s) line (see Figure 5). Advance the needle slowly through the posterior lumbar fascia, paraspinous muscles, anterior lumbar fascia, quadratus lumborum and into the psoas muscle. Passage through these fascial layers may be detected by distinct “pops” when using a short bevelled needle. Using a nerve stimulator quadriceps muscle twitches in the ipsilateral thigh are sought. If hamstring contractions are observed, direct the needle laterally. If hamstring and quadriceps contractions are observed simultaneously, direct the needle more cephalad to isolate the lumbar plexus rather than sacral plexus.[26],[27]
The depth from the skin to the lumbar plexus is approximately the same distance as the posterior superior iliac spine is to the intercristal line.27The depth of the needle is emphasized because complications include renal haematoma, vascular puncture (retroperitoneal haematoma) or even bowel puncture.
Femoral nerve block
Position:
Supine, foot rotated outward.
Landmarks:
Femoral pulse, inguinal ligament.
Dose:
0.2-0.3ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine.
Femoral nerve blocks are most useful in cases of fractured femur, and allow painless transport, radiographic examination and application of splints.[23],[28],[29] Most lower limb surgery can be performed when femoral nerve block is used in combination with sciatic nerve or lateral cutaneous nerve of thigh block. For surgery on the knee it is best used in combination with a sciatic nerve block.[23],[30]
Technique:
The femoral nerve may be blocked as it emerges from below the inguinal ligament in the femoral canal lateral to the femoral artery in the femoral triangle. Although a femoral nerve block can be performed without a nerve stimulator (e.g. for unsedated children with femoral fractures to avoid pain caused by muscle contractions) greater success can be achieved using one.
Insert the needle approximately 0.5-1cm lateral to the femoral pulsation and approximately 0.5-1cm below the inguinal ligament. It is useful to map the course of the femoral nerve prior to inserting the needle.[8]
The nerve lies beneath the fascia lata and fascia iliaca and often two distinct ‘pops’ are felt as needle traverses these layers. Quadriceps contraction confirms femoral nerve stimulation but should not be confused with direct stimulation of the sartorius muscle. Local anaesthetic should be easy to inject into the femoral canal. Resistance to injection suggests intraneural injection.
“3 in 1” block
A “3 in 1” block is essentially a femoral nerve block that attempts to anaesthetize the femoral, lateral cutaneous nerve of thigh and obturator nerves with one injection by causing retrograde spread of local within the femoral sheath up to the lumbar plexus by applying digital pressure distal to the injection site. It is only 20% effective in blocking all three nerves.31 All three nerves are more reliably blocked with a fascia iliaca or a lumbar plexus block.
Lateral femoral cutaneous nerve of thigh
Indications:
To provide analgesia for plating of the femur, plate removal, drainage of femoral osteitis, harvesting skin grafts or muscle biopsies.
Position:
Supine.
Landmarks:
Anterior superior iliac spine, inguinal ligament.
Dose:
1-3ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
Anatomy:
The lateral cutaneous nerve of thigh is derived from the lumbar plexus (L2-L3) and is purely sensory supplying the anterolateral aspect of the thigh. The nerve descends over the iliacus muscle just below the pelvic rim in an aponeurotic canal formed in the fascia lata and enters the thigh close to the anterior superior iliac spine (ASIS) behind the inguinal ligament. In the thigh it crosses or passes through the tendinous origin of the sartorius muscle. It divides into anterior and posterior branches.
Technique: Insert a needle 1-2 cm below and medial to the origin of the inguinal ligament at the anterior superior iliac spine until a ‘pop’ is felt as the fascia lata is penetrated and a second ‘pop’ when the fascia iliaca is entered. If bone contact is made, the needle should be withdrawn and redirected. Correct placement of the needle can also be determined with a loss of resistance technique noted as the fascia iliaca compartment is entered.
Fascia iliaca compartment block
Indications:
This block is particularly useful for any surgery performed on the lower extremity above the knee and for femoral shaft fractures. The fascia iliaca compartment block was originally described in children by Dalens and is more effective in blocking the femoral, lateral cutaneous nerve of thigh and obturator nerves than the “3-in-1”block.[31]
Position:
Supine.
Landmarks:
ASIS, inguinal ligament, pubic tubercle.
Dose:
0.5-1ml.kg-1 0.25-0.5% bupivacaine, or 1-2% lignocaine.
Technique:
With the child in the supine position and the thigh slightly abducted and externally rotated, draw a line from the pubic tubercle to the ASIS along the inguinal ligament. Insert a needle perpendicular to the skin 0.5-1cm below the junction of lateral and middle third of this line. Two “pops” are felt as the needle pierces the fascia lata and then the fascia iliaca. Larger volumes are required because the aim is to block all three nerves with one injection. Massaging the area in an upward direction may facilitate the upward spread of local anaesthetic. No significant complications are seen provided that the needle remains (below) inferior to the inguinal ligament and away from the femoral vessels.
Sciatic nerve block
The sciatic nerve leaves the posterior pelvis via the greater sciatic foramen through the piriformis muscle into the buttock and descends in the midline of the leg posteriorly to the apex of the popliteal fossa. The sciatic nerve lies midway between the greater trochanter and the ischial tuberosity at the gluteal cleft where it is palpable in most young children.[6] The sciatic nerve divides into the common peroneal and the tibial nerve within the popliteal fossa in the majority of children.[32]
The sciatic nerve can be blocked using several different approaches at the hip or in the popliteal fossa.[32],[33],[34],[35] The approach chosen ultimately determines the distribution of motor and sensory blockade. Sciatic nerve block at the gluteal level provides anaesthesia for the posterior aspect of the thigh and leg below the knee but excludes the medial aspect of the lower half of the leg, the medial malleolus and the medial aspect of the foot.
Indications:
All surgical procedures involving the posterior aspect of the leg especially below the knee, for example lengthening of the Achilles tendon, uni- or bilateral club foot repair as well as for major foot arthrodesis.6 It may need to be supplemented with other blocks depending on the type of surgery, for example knee surgery or tibial osteotomies. The different approaches to the sciatic nerve in children are described below.
Posterior approach to the sciatic nerve
Position:
Lateral recumbent, hip flexed, knee flexed, the side to be blocked uppermost.
Landmarks:
Coccyx, greater trochanter, ischial tuberosity.
Dose:
0.2-0.3ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine.
Technique:
With the child in position, draw a line from the tip of the coccyx to the greater trochanter. Insert a needle at the midpoint of this line and direct towards the ischial tuberosity. A nerve stimulator, set at 0.3 to 0.4mA, will elicit distal motor responses in the leg or foot confirming stimulation of the sciatic nerve (which supplies all the muscles below the knee).
Infragluteal approach to the sciatic nerve
Position:
Supine or lateral decubitus, hip flexed, knee extended.
Landmarks:
Greater trochanter, ischial tuberosity, gluteal crease, biceps femoris muscle.
Dose:
0.2-0.3ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
Technique:
A useful technique in children has been described by Raj.[6],[35] Insert a needle posteriorly perpendicular to the skin at a point midway between the ischial tuberosity and greater trochanter on the gluteal crease. With exaggerated hip flexion the glutei may be flattened and the sciatic nerve becomes relatively superficial even in some obese children. The nerve is often palpable in the groove lateral to biceps femoris in young children. Plantar flexion, inversion or dorsi-flexion at 0.3-0.4 mA confirms sciatic nerve stimulation. The posterior cutaneous nerve of the thigh may be missed since the nerve may separate more proximally in the thigh.
Anterior approach to the sciatic nerve
Position:
Supine, hip and knee extended
Landmarks:
pubic tubercle, anterior superior iliac spine, greater trochanter
Dose:
0.2-0.3ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
Technique:
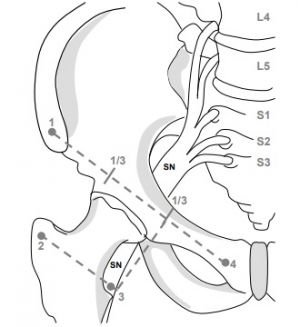
(see Figure 6). A line drawn from the pubic tubercle to the anterior superior iliac spine (inguinal ligament) is divided into thirds. A perpendicular is then dropped from the junction of the inner and middle thirds onto a line drawn parallel to the inguinal ligament through the greater trochanter. This point corresponds approximately with the lesser trochanter below.
Posterior mid-thigh approach to the sciatic nerve
Position:
Supine, hip flexed, knee flexed or extended.
Landmarks:
Ischial tuberosity, head of fibula.
Dose:
0.2-0.3ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
Technique:
Insert a needle perpendicular to the midpoint of a line drawn from the head of fibula to the ischial tuberosity in the posterior thigh. The nerve is surrounded by the hamstring muscles at this point and this compartment can be located using a loss of resistance technique or by nerve stimulation that produces a motor response in the ankle, foot or big toe.[36] The posterior cutaneous nerve of thigh is missed at this level.
Sciatic nerve in the popliteal fossa
Position:
Prone, lateral or supine.
Landmarks:
Apex-popliteal fossa.
Dose:
1-2ml 0.25-0.5% bupivacaine or 1-2% lignocaine.
The sciatic nerve may be blocked as it courses through the popliteal fossa behind the knee for procedures of the distal lower extremity.[36],[37],[38]The popliteal fossa is formed by the semimembranosus and semitendinosus tendons medially, the biceps femoris tendon laterally, and the popliteal crease between the femoral condyles inferiorly.
The sciatic nerve divides in the vicinity of popliteal fossa into two branches - the common peroneal and the posterior tibial nerves. The exact location of this division is variable but in the majority of children it is within the popliteal fossa.[32],[39] The common peroneal nerve courses laterally medial to the biceps femoris tendon before passing over the lateral head of gastrocnemius and around the head of the fibula. The posterior tibial nerve courses down the midline of the lower leg posteriorly in close proximity, but superficial to the popliteal artery within the popliteal fossa.
Although the nerves branch, there is a common epineural sheath that envelops both the posterior tibial and the common peroneal nerve.[38] For this reason a high rate of success can be achieved even when the motor response of only one branch is elicited. Stimulation of the common peroneal will cause dorsiflexion and eversion of the foot while stimulation of the posterior tibial nerve will elicit inversion and plantar flexion. (Internal nerve, i.e. posterior tibial nerve - Inversion; External nerve i.e. common peroneal nerve - Eversion). The nerves can be “mapped” individually particularly in young infants.
Various landmarks have been described for the insertion of the needle. For each 10kg body weight the needle insertion moves 1cm further above the popliteal crease just lateral to the midline.[32] Alternatively, insert a needle at the apex of the popliteal fossa to block both the posterior tibial and common peroneal nerve.
Complications are rare but take care to avoid intravascular injection.
Lateral approach to the sciatic nerve at the knee
Position:
Supine.
Landmarks:
Biceps femoris tendon.
Dose:
0.1ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine.
A lateral approach to the popliteal fossa has recently been described in children.[40] Identify the biceps femoris tendon on the postero-lateral aspect of the knee approximately 4-6 cm above the popliteal crease. Insert a needle anterior to the biceps femoris tendon until the needle contacts the shaft of the femur. At this point gently walk the needle off the femur posteriorly and advance until foot dorsiflexion or plantar flexion along with eversion is elicited.
Saphenous nerve block
Indication:
The main indication for blocking this nerve is to compliment a sciatic nerve block for surgery on the medial aspect of the lower limb or foot.
Position:
Supine.
Landmarks:
Femoral artery, sartorius, inguinal ligament.
Dose:
0.1-0.2ml.kg-1 0.25-0.5% bupivacaine or1-2% lignocaine.
The saphenous nerve runs along the medial aspect of the thigh just lateral to and within the same fascial sheath as the motor nerve supplying the vastus medialis.
The nerve to vastus medialis can be located using a nerve stimulator. Insert an insulated needle perpendicular to the skin 0.5cm lateral to the point where the femoral artery crosses the medial border of the sartorius muscle in the anterior thigh. Muscle twitches in the sartorius muscle confirm the close proximity to the saphenous nerve at this level. The distance from the inguinal ligament (3-5cm) varies with age, as does the depth of the nerve (0.5-3cm).
An advantage of this block over a femoral block is that motor activity in the remainder of the quadriceps is spared.
The saphenous nerve is a purely sensory nerve at the knee. At the level of the tibial plateau the saphenous nerve perforates the fascia lata between the sartorius and gracilis where it lies subcutaneously in close proximity to the long saphenous vein.
Make a deep linear subcutaneous infiltration below and behind the insertion of the sartorius tendon (medial surface of tibia) where the nerve lies in a shallow gutter immediately in front of the upper part of the medial head of gastrocnemius. Intermittent aspiration will reduce the risk of injection into the long saphenous vein.
Ankle block
Position:
Supine or prone.
Landmarks:
Medial and lateral malleolus, extensor hallucis longus tendon, Achilles tendon, dorsalis pedis pulse.
Dose:
0.1ml.kg-1 0.25-0.5% bupivacaine or 1-2% lignocaine.
Ankle blocks are used for procedures confined to the foot including distal phalangeal amputations, foreign body removal and simple reconstructive surgery. The five peripheral nerves blocked at this level are the terminal branches of the sciatic (posterior tibial, superficial peroneal, deep peroneal and sural nerves) and femoral (saphenous) nerves.
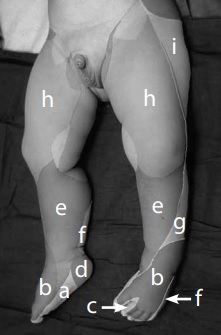
An ankle block is relatively easy to perform by injecting a subcutaneous ring at the ankle. Avoid local anaesthetics containing adrenaline since it may compromise end-arteries in the foot. Block each nerve separately for best results (see Figure 7).
- (a) The tibial nerve innervates the sole of the foot and medial aspect of the heel and lies between the medial malleolus and the calcaneum deep to the flexor retinaculum immediately posterior to the posterior tibial artery. Local anaesthetic injected through a needle inserted posteromedially to the Achilles tendon and directed towards the arterial pulsation should block the tibial nerve.
- (b) The superficial peroneal nerve supplies the dorsum of the foot and is blocked by a subcutaneous injection across the dorsum of the foot between the lateral malleolus and the extensor hallucis longus tendon.
- (c) The deep peroneal nerve innervates the first web space between the 1st and 2nd toe. Insert a needle medial to extensor hallucis longus tendon along anterior tibial arterial pulsation until it contacts the tibia. Withdraw the needle a few millimetres and inject the local anaesthetic solution.
- (d) The sural nerve innervates the lateral aspect of the foot. Introduce a needle posterio-lateral to the Achilles tendon between the lateral malleolus and the calcaneum until bony contact is made. Withdraw the needle a few millimetres and inject the local anaesthetic solution.
- (e) The saphenous nerve innervates the medial aspect of the ankle and foot and lies in close proximity to the saphenous vein. It is located on the medial side of the dorsum of the foot anterior to the medial malleolus. A subcutaneous injection from the medial malleolus along the anterior aspect of the ankle towards the saphenous vein will block the nerve.
SAFE CONDUCT OF PERIPHERAL NERVE BLOCKS
Patients should be carefully monitored whilst nerve blocks are performed. This should include ECG, BP and pulse oximetry. Resuscitation equipment (oxygen, anticonvulsants, Ambu bag and Intralipid) should be available in the event of local anaesthetic toxicity or anaphylaxis. (See Table 3)
| Management of systemic toxicity[41],[42] |
|---|
| Airway - Maintain the patient’s airway, administer 100% oxygen |
| Breathing - Start ventilation: if breathing inadequate intubate |
| Circulation - Pulse check: if cardiac arrest, start CPR. |
| Convulsions - IV diazepam, 1-3mg.kg-1 thiopentone, muscle relaxation prn |
| Hypotension - Ephedrine 3-6mg increments, elevate legs, IV fluid bolus |
| Intralipid 20% - 1-1.5ml.kg-1 followed by infusion 0.25ml.kg-1.min-1 |
CONCLUSION
Expertly performed, peripheral nerve blocks can provide long lasting anaesthesia and analgesia for surgery or after injury to the upper or lower limbs in children. Specific knowledge is required for the indication, technique and dose of local anaesthetic for each block. Accuracy is improved if a nerve stimulator or ultrasound guidance is used. A safe dose of local anaesthetic must be used at all times, and care taken to avoid inadvertent intravascular injection of local anaesthetic. Additional information and video descriptions of peripheral nerve blocks can be obtained from the Internet, for instance from the New York School of Anaesthesia website: http://+www.nysora.com/
REFERENCES
- ↑ Suresh S, Wheeler M. Practical pediatric regional anesthesia. Anesthesiol. Clin.North America 2002; 20: 83-113.
- ↑ Ross AK, Eck JB, Tobias JD. Pediatric regional anesthesia: beyond the caudal. Anesth Analg 2000; 91: 16.
- ↑ Giaufre E, Dalens B, Gombert A. Epidemiology and morbidity of regional anesthesia in children: A one-year prospective survey of the French-language society of pediatric anesthesiologists. Anesth Analg 1996; 83: 904-12.
- ↑ Polaner DM, Taenzer AH, Walker BJ et al. Pediatric Regional Anaesthesia Network (PRAN): A Multi-Institutional Study of the Use and Incidence of Complications of Pediatric Regional Anaesthesia. Anesth Analg 2012; 22: 115-9
- ↑ Ecoffey C, Lacroix F Giaufré E et al. Epidemiology and morbidity of regional anaesthesia in children: a follow-up one-year prospective survey of the French- Language Society of Paediatric Anaesthesiologists (ADARPEF). Pediatr Anesth 2010; 20: 1061-9.
- ↑ 6.0 6.1 6.2 Bosenberg AT. Lower limb blocks in children using unsheathed needles and a nerve stimulator. Anaesthesia 1995; 50: 206-10.
- ↑ Hadzic A. Peripheral nerve stimulators: cracking the code – one at a time. Reg Anesth Pain Med 2004; 29: 185-8.
- ↑ 8.0 8.1 Bosenberg AT, Raw R, Boezaart AP: Surface mapping of peripheral nerves in children with a nerve stimulator. Paediatr. Anaesth 2002; 12: 398-403.
- ↑ Chan V: Advances in regional anaesthesia and pain management. Can.J Anaesth. 1998; 45: R49-63
- ↑ 10.0 10.1 Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth 2005; 94: 7-17.
- ↑ 11.0 11.1 Tsui B, Suresh S. Ultrasound imaging for regional anaesthesia in infants, children, and adolescents: a review of current literature and its application in the practice of extremity and trunk blocks. Anesthesiology 2010; 112: 473-92.
- ↑ 12.0 12.1 12.2 12.3 Marhofer P, Willschke H, Kettner S. Ultrasound-guided upper extremity blocks-tips and tricks to improve the clinical practice. Pediatr Anesth 2012; 22: 65-71.
- ↑ 13.0 13.1 13.2 Sites BD, Chan VW, Neal JM et al. The American Society of Regional Anaesthesia and Pain Medicine and the European Society of Regional Anaesthesia and Pain Therapy joint committee recommendations for education and training in ultrasound-guided regional anaesthesia. Reg Anesth Pain Med 2010; 35: S74-80.
- ↑ 14.0 14.1 14.2 . Tobias JD. Brachial plexus anaesthesia in children. Paed Anaesth 2001; 11: 265.
- ↑ Carre P, Joly A, Field BC, et al. Axillary block in children: single or multiple injection? Paed Anaesth 2000; 10: 35-9.
- ↑ 16.0 16.1 Cramer KE, Glasson S, Mencio G, Green NE: Reduction of forearm fractures in children using axillary block anesthesia. J.Orthop. Trauma 1995; 9: 407-10.
- ↑ 17.0 17.1 Fisher WJ, Bingham RM, Hall R. Axillary brachial plexus blocks for perioperative analgesia in 250 children. Paediatr Anaesth 1999; 9: 435-8.
- ↑ 18.0 18.1 18.2 . Kilka HG, Geiger P, Mehrkens HH: Infraclavicular vertical brachial plexus blockade. A new method for anesthesia of the upper extremity. An anatomical and clinical study Anaesthesist 1995; 44: 339-44.
- ↑ 19.0 19.1 Dadure C, Raux O, Troncin R, Rochette A, Capdevila X: Continuous infraclavicular brachial plexus block for acute pain management in children. Anesth Analg. 2003; 97: 691-3.
- ↑ 20.0 20.1 20.2 Fleischman E, Marhofer P, Greher M et al. Brachial plexus anaesthesia in children: lateral infraclavicular vs axillary approach. Paediatr Anaesth 2003; 13:103-8
- ↑ 21.0 21.1 . Marhofer P, Sitzwohl C, Greher M et al. Ultrasound guidance for infraclavicular brachial plexus anaesthesia in children. Anaesthesia 2004; 59: 642-46.
- ↑ Dalens B, Vanneuville G, Tanguy A. A new parascalene approach to the brachial plexus in children: comparison with the supraclavicular approach. Anesth Analg 1987; 66: 1264-71
- ↑ 23.0 23.1 23.2 Tobias JD. Regional anaesthesia of the lower extremity in infants and children. Paediatr Anaesth 2003; 13:152-63.
- ↑ McLeod DH, Wong DH, Claridge RJ, Merrick PM: Lateral popliteal sciatic nerve block compared with subcutaneous infiltration for analgesia following foot surgery. Can.J.Anaesth. 1994; 41: 673-6.
- ↑ Tobias JD, Mencio GA. Popliteal fossa block for postoperative analgesia after foot surgery in infants and children. J Pediatr Ortho 1999; 19: 511-4.
- ↑ Dalens B, Tanguy A, Vanneuville G. Lumbar plexus block in children: a comparison of two procedures in 50 patients. Anesth Analg 1988; 67: 750-8.
- ↑ . Walker BJ, Flack SH, Bosenberg AT. Predicting lumbar plexus depth in children and adolescents. Anesth Analg. 2011; 112: 661-5.
- ↑ Ronchi L, Rosenbaum D, Athouel A, et al. Femoral nerve blockade in children using bupivacaine. Anesthesiology 1989; 70: 622-4.
- ↑ Tobias JD: Continuous femoral nerve block to provide analgesia following femur fracture in a paediatric ICU population. Anaesth Intensive Care 1994; 22: 616-8.
- ↑ . Reuben SS, Sklar J: Pain management in patients who undergo outpatient arthroscopic surgery of the knee. J Bone Joint Surg Am. 2000; 82-A: 1754-66.
- ↑ Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg 1989; 69: 705-13.
- ↑ 32.0 32.1 32.2 32.3 . Konrad C, Johr M. Blockade of the sciatic nerve in the popliteal fossa: a system for standardization in children. Anesth Analg 1998; 87: 1256-8.
- ↑ Dalens B, Tanguy A, Vanneuville G. Sciatic nerve blocks in children: comparison of the posterior, anterior, and lateral approaches in 180 pediatric patients. Anesth Analg 1990; 70: 131-7.
- ↑ . Sukhani R, Candido KD, Doty R, et al. Infragluteal-parabiceps sciatic nerve block: an evaluation of a novel approach using a single-injection technique. Anesth Analg. 2003; 96: 868-73.
- ↑ 35.0 35.1 Raj PP, Parks RI, Watson TD, et al. A new single-position supine approach to sciatic-femoral nerve block. Anesth Analg 1975; 54: 489-94.
- ↑ 36.0 36.1 . Kempthorne PM, Brown TCK. Nerve blocks around the knee in children. Anaesth Intens Care 1984; 12: 14-17
- ↑ Tobias JD, Mencio GA. Popliteal fossa block for postoperative analgesia after foot surgery in infants and children. J Pediatr Ortho 1999; 19: 511.
- ↑ 38.0 38.1 Vloka JD, Hadzik A, Lesser JB, et al. A common epineural sheath for the nerves in the popliteal fossa and its possible implications for sciatic nerve block. Anesth Analg 1997; 84: 387-90
- ↑ Schwemmer U, Markus CK, Greim CA, Brederlau J, Trautner H, Roewer N: Sonographic imaging of the sciatic nerve and its division in the popliteal fossa in children. Pediatr.Anesth 2004; 14:1005-8.
- ↑ terRahe CT, Suresh S: Popliteal fossa block: Lateral approach to the sciatic nerve. Tech in Reg Anesth Pain Management 2002; 6:141-3.
- ↑ Neal JM, Bernards CM, Butterworth JF et al ASRA Practice Advisory on Local Anesthetic Systemic Toxicity. Reg Anesth Pain Med 2010; 35: 152-61
- ↑ Harclerode Z, Michael S. Axillary brachial plexus block landmark techniques. Tutorial of the Week 165 (January 2010)